The prostate is a walnut-sized gland in men that is part of the reproductive system.
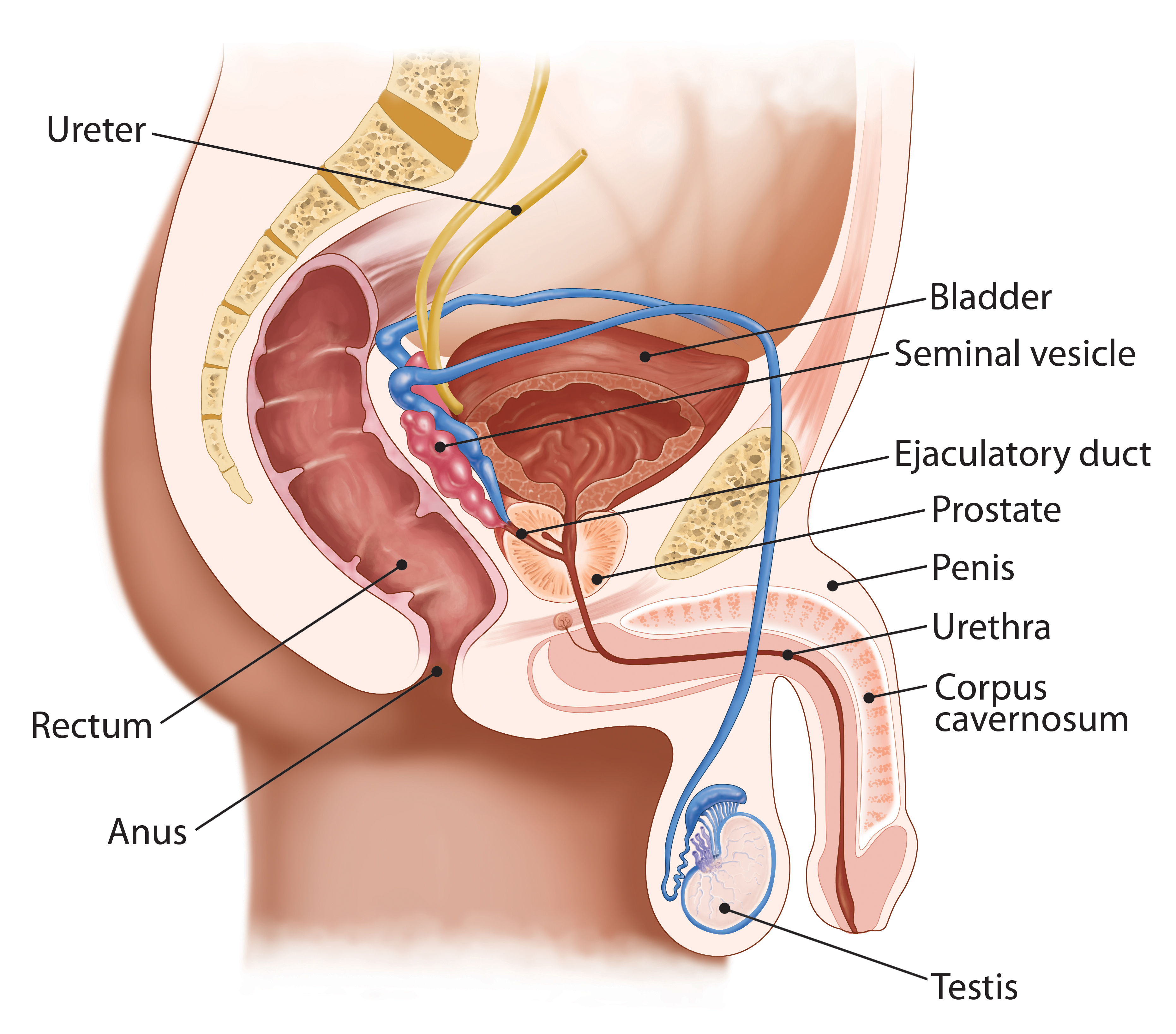
The prostate sits low in the pelvis, below the bladder, in front of the rectum and the prostate surrounds the urethra. The prostate makes seminal fluid, the liquid in sperm that protects, supports and helps transport sperm.
Chemotherapy
Gleason Score
Prostate Cancer Grading & Prognostic Scoring
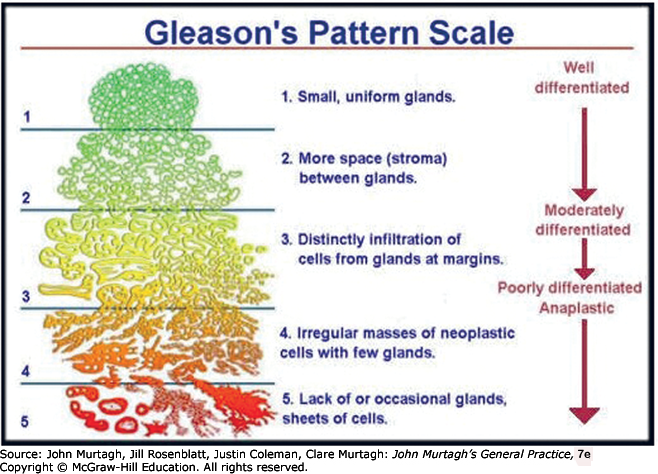
The Gleason Score is the grading system used to determine the aggressiveness of prostate cancer. This grading system can be used to choose appropriate treatment options.
The Gleason Score ranges from 1-5 and describes how much the cancer from a biopsy looks like healthy tissue (lower score) or abnormal tissue (higher score). Most cancers score a grade of 3 or higher.
Since prostate tumors are often made up of cancerous cells that have different grades, two grades are assigned for each patient. A primary grade is given to describe the cells that make up the largest area of the tumor and a secondary grade is given to describe the cells of the next largest area. For instance, if the Gleason Score is written as 3+4=7, it means most of the tumor is grade 3 and the next largest section of the tumor is grade 4, together they make up the total Gleason Score. If the cancer is almost entirely made up of cells with the same score, the grade for that area is counted twice to calculated the total Gleason Score.
Typical Gleason Scores range from 6-10. The higher the Gleason Score, the more likely that the cancer will grow and spread quickly.
- Scores of 6 or less describe cancer cells that look similar to normal cells and suggest that the cancer is likely to grow slowly.
- A score of 7 suggests and intermediate risk for aggressive cancer. Scoring a 7 means that the primary score (largest section of the tumor) scored a 3 or 4. Tumors with a primary score of 3 and a secondary score of 4 have a fairly good outlook, whereas cancers with a primary Gleason Score of 4 and a secondary score of 3, are more likely to grow and spread.
- Scores of 8 or higher describe cancers that are likely to spread more rapidly, these cancers are often referred to as poorly differentiated or high grade.
How Important is the Gleason Score?
The Gleason Score is very useful for predicting the behavior of a prostate cancer. However, other factors also contribute to determining the stage of prostate cancer, including:
- The PSA level
- Findings from a rectal exam
- The number of biopsy core samples that contain cancer
- The percentage of cancer making up each biopsy core sample
- If cancer is found in one or both sides of the prostate
- If the cancer has spread outside the prostate
FAQ
How Important Is the Gleason Score?
The Gleason Score is very important in predicting the behavior of a prostate cancer. Still, other factors are also important such as:
- The PSA Level
- Findings on a rectal exam
- How much of each core is made up of cancer
- The number of cores that contain cancer
- Whether cancer was found in both sides of the prostate
- Whether the cancer has spread outside the prostate
What does it mean to have a Gleason Score of 6 or 7 or 8-10?
The lowest Gleason Score of a cancer found on a prostate biopsy is 6. These cancers may be called well-differentiated or low-grade and are likely to be less aggressive - they tend to grow and spread slowly.
Cancers with Gleason Scores of 8 to 10 may be called poorly differentiated or high grade. These cancers tend to be aggressive, meaning they are likely to grow and spread more quickly.
Cancers with a Gleason Score of 7 may be called moderately differentiated or intermediate grade. The rate at which they grow and spread tends to be in between the other 2.
My Gleason Score Looks Different
Other ways that this Gleason Score may be listed in your report are Gleason 7/10, Gleason 7 (3+4) or combined Gleason Grade of 7.
What does it mean when there are different core samples with different Gleason Scores?
Cores may be samples from different areas of the same tumor or different tumors in the prostate. Because the grade may vary within the same tumor or between different tumors, different samples (cores) taken from your prostate may have different Gleason Scores. Typically, the highest (largest number) Gleason Score will be the one used by your doctor for predicting your prognosis and deciding treatment.
Can the Gleason Score on my biopsy really tell what the cancer grade is in the entire prostate?
Prostate biopsies are tissue samples from different areas of the prostate. The Gleason Score on a biopsy usually reflects the cancer's true grade. However, it is possible that the Gleason Score from your biopsy is lower or higher than the true grade. To reduce the risk of over-or-under scoring, multiple biopsies are usually taken from different areas within the prostate.
What does it mean if my biopsy mentions that there is perineural invasion?
Perineural invasion means that cancer cells were seen surrounding or tracking along a nerve fiber with the prostate. When this is found on a biopsy, it means there is a higher chance that the cancer has spread outside the prostate. Still, perineural invasion does not mean that the cancer has spread, and other factors, such as the Gleason Score and amount of cancer in the cores are more important. In some cases, findings perineural invasion may affect treatment, so if your report mentions perineural invasion, you should discuss it with your doctor.
What does it mean if my biopsy report also says high-grade prostatic intraepithelial neoplasia or high-grade PIN?
High-grade prostatic intraepithelial neoplasia (or high-grade PIN) is a pre-cancer to the prostate. In this instance, high-grade refers to the PIN and not the Gleason Score.
What does it mean if, in addition to cancer, my biopsy report also says atypical glands or atypical small acinar proliferation (ASAP) or glandular atypia or atypical grandular proliferation?
All of these terms mean the pathologist saw something in your biopsy that suggests cancer may be present, but they cannot be certain. For individuals with known prostate cancer this is no longer relevant.
What does it mean if in addition to cancer my biopsy report also says acute inflammation (acute prostatitis) or chronic inflammation (chronic prostatitis)?
Inflammation of the prostate is called prostatitis. Most cases of prostatitis reported on a biopsy are not caused by infection and do not need to be treated. In some cases, inflammation may increase you PSA level, but it is not linked to prostate cancer. The finding of prostatitis on a biopsy of someone with cancer does not affect their prognosis or the way the cancer is treated.
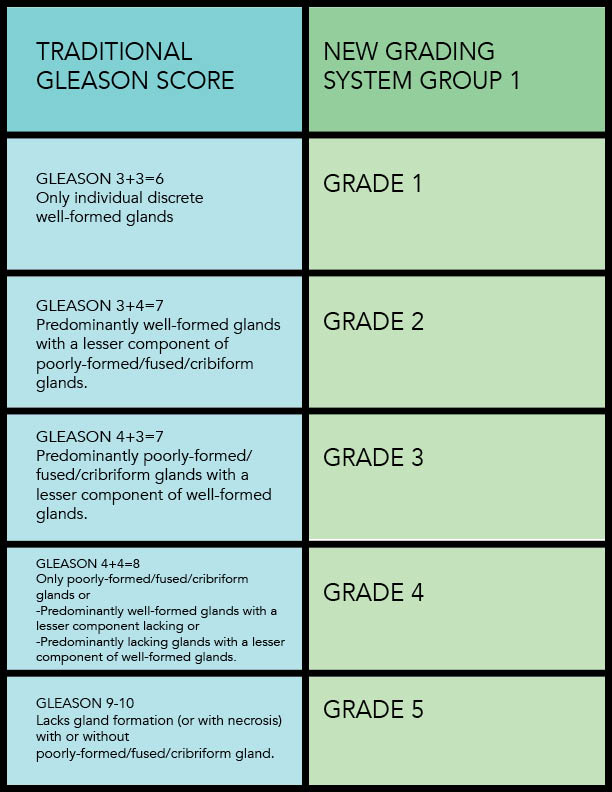
New Prostate Cancer Grading System: The new prostate grading system is an extension of the current Gleason grading scale for determining the stage of prostate cancer. This system is designed to provide a simplified and more accurate grading stratification system than the current Gleason Score. This new method is especially focused on better representing low grade disease to reduce unnecessary treatment of indolent prostate cancer. The new grading system subdivides prostate cancer into five categories using pathological characteristics as described in the table below.
Staging
AJCC TNM Staging
American Joint Committee on Cancer (AJCC) TNM Staging
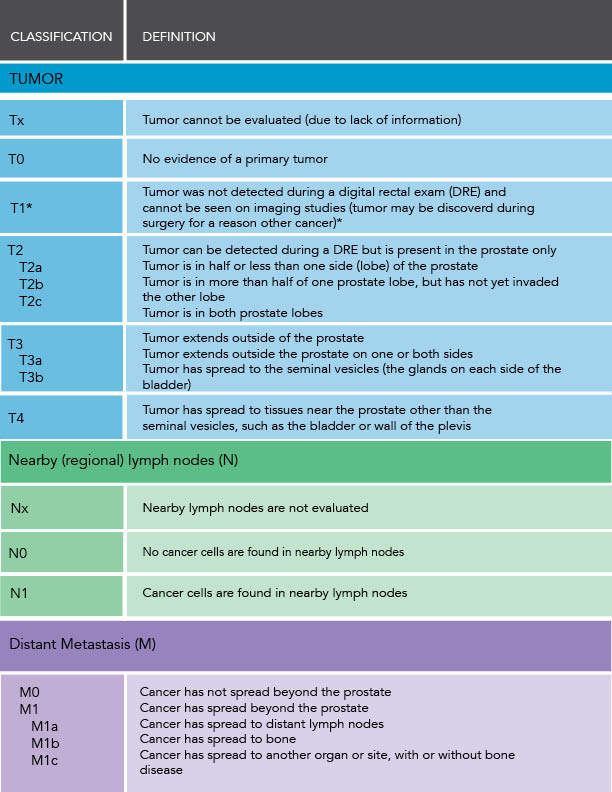
A staging system is a standard method for the cancer care team to describe how far a cancer has spread. The TNM system is based on 5 key pieces of information:
1. The size and extent of the primary Tumor (T category)
- T1 - The tumor is not detectable with a digital rectal exam (DRE) or imaging but is found in prostate tissue from a biopsy or surgical treatment.
- T1a - Cancer is found in 5% or less of the removal tissue.
- T1b - Cancer is found in more than 5% of the removed tissue.
- T1c - Tumors are found by needle biopsy done for a high PSA. - T2 - The tumor is detectable with a DRE or imaging but is confined to the prostate.
- T2a - Cancer is in no more than one half of one side of the prostate.
- T2b - Cancer is in more than half of one side of the prostate.
- T2c - Cancer is in both sides of the prostate. - T3 - Cancer has grown outside the prostate and may have grown into the seminal vesicles.
- T3a - Cancer has spread outside the prostate but not to the seminal vesicles.
- T3b - Cancer has spread to the seminal vesicles. - T4 - Cancer has grown into other nearby tissues, such as the urethral sphincter, rectum, bladder or wall of the pelvis.
2. Whether the cancer has spread to nearby lymph Nodes (N Category)
- NX - The lymph nodes have not been assessed for cancer.
- N0 - There is no cancer in nearby lymph nodes.
- N1 - Cancer has spread to nearby lymph nodes.
3. The absense or presence of cancer outside the prostate, or Metastasis (M Category)
- MX - It is unknown if cancer has spread to distant sites.
- M0 - The cancer has not spread to distant sites.
- M1 - Cancer has spread to distant sites.
- M1a - Cancer has spread to distant lymph nodes.
- M1b - Cancer has spread to bones.
- M1c - Cancer has spread to distant organs.
4. The PSA level at the time of diagnosis.
Prostate-specific antigen, or PSA, is a protein produced by cells of the prostate gland. The PSA test measures the level of PSA in a man's blood. PSA is present in small quantities in the serum of men with healthy prostates, but is often elevated in the presence of prostate cancer or other prostate disorders.
Taken together, this information is used to determine the overall staging for a patient's prostate cancer. The stage is usually expressed in Roman numerals from I (the least advanced) to IV (the most advanced). The AJCC TNM staging system is the most widely used system for prostate cancer and is very important for treatment planning. This information is summarized in the table below.
There are two types of staging for prostate cancer, the first is the clinical stage, which is determined based on the results of a physical exam (including DRE), lab tests, prostate biopsy and imaging tests. The second type of staging is the pathologic stage, which incorporates information gathered during an examination of prostate tissue removed during surgery. Pathologic staging is likely to be more accurate than clinical staging, as it allows for assessment of the prostate tissue. If you have not undergone surgery, your doctor will use the clinical staging method to assess your cancer risk. For patients who have undergone a surgical resection of the prostate, your doctor will use the pathologic staging method and will incorporate information obtained from analysis of your prostate tissue into your diagnosis. This is one possible advantage of having surgery (radical prostatectomy) as opposed to radiation therapy or active surveillance.
Biopsies
If a patient has an elevated PSA test result and/or an abnormal DRE the physician may recommend a biopsy of the prostate.
A diagnosis of prostate cancer is achieved through an ultrasound-guided biopsy of the prostate gland. A prostate biopsy is conducted with a transrectal ultrasound and biopsy needle to collect small slivers of prostate tissue that are analyzed for cancer. This tissue is then examined under a microscope for cancer cells. A biopsy of the prostate can be performed in the physician’s office and patients usually return home the same day. Keep in mind that it is still possible to have cancer, even if the biopsy is negative, because the cancer cells may not have progressed enough to be detected by a microscope or the biopsy may miss the areas of cancer within the prostate.
Core Needle Biopsy
Once it has been determined that a patient is a candidate for prostate biopsy, how is this performed? Since the late 1980's, the standard for prostate biopsy has been under the direction of the urologist utilizing trans rectal ultrasound (TRUS) and needle biopsy obtained directly through the wall of the rectum via the US probe. This technique does not require general anesthesia and can be performed with local anesthesia or sedation in an office setting or ambulatory surgery center. The TRUS allows the urologist to measure the size of the prostate and arbitrarily divide the gland into six distinct areas where 2 biopsies are taken from each. For the most part the majority of the time, the TRUS is not identifying an abnormality but merely allowing the provider to segment the prostate gland. Thus, the procedure is a systematic approach but the biopsies are randomly taken in the six areas and termed sextant biopsy.
Advances in prostate MRI technology has gained prominence over the past 10 years and although not always offered in some parts of the U.S., the general workflow is that a prostate mpMRI is ordered by the urologist if there is a suspicion that an aggressive tumor may be present. This is obtained prior to biopsy and generally performed in a dedicated imaging center. It is critical that a qualified and experienced radiologist interpret the study to determine if there are regions of interest. These lesions are assigned a score of 1 - 5, based on the Prostate Imaging-Reporting and Data System (PI-RADS). At this point, the patient is referred back to the urologist where a biopsy can be performed using one of two techniques:
1. Cognitive Fusion of the prostate, U/S guided
2. Mechanical Fusion of the prostate with co-registration, U/S guided.
Both utilize the traditional TRUS sextant biopsy technique described above. If the radiologist has identified regions of interest, the former method involves the urologist looking at the MRI and placing the biopsy needles in the area that he believes correlates what he is seeing on U/S. The latter technique requires a third piece of hardware, the registration unit. This unit is in the room with the urologist at the time of biopsy, imports the MRI from the imaging center, imports the U/S image from the urologist real time and superimposes or "fuses" the 2 together. So now it appears the urologist is taking his biopsies from the MRI image, especially with regions of interest. Clearly this represents a much more precise way of performing a prostate biopsy. Unfortunately, the utilization of mpMRI is not always available.
In about 50% of the cases, the biopsy comes back as negative and no cancer. As we previously discussed, the traditional sextant TRUS, the current standard of care for prostate biopsy, only samples about 1% of the total gland. So a negative biopsy does not mean that there is no cancer and thus urologists continue to follow PSA values.
Mapping Biopsy
A mapping biopsy is very similar to the standard TRUS needle biopsy described above. However, a mapping biopsy removes many more core samples and is performed as an outpatient procedure under general anesthesia. A physician places a grid below the patient's scrotum and takes between 35-80 biopsies of the prostate. This procedure allows the entire prostate to be biopsied and results in the creation of a three-dimensional image of the prostate, including the location of cancer within the gland. This biopsy may be better for determining the size and location within the prostate, and allow for patients and physicians to more appropriately select treatment options. This method of biopsy may help to eliminate errors in the grading of prostate cancer and unnecessary treatments.
Side Effects
As with any medical procedure biopsies can have side effects. Patients may be given antibiotics to take before or after the biopsy to reduce the risk of infection. The following are some common side effects of a prostate biopsy:
- Soreness
- Blood in urine or semen
- Rectal bleeding
- Infection
Imaging
An imaging test uses sound waves, radioactive particles, or magnetic fields to create an image. These images allow physician to see changes in the body that may be caused by cancer. Imaging is an essential component in the treatment of prostate cancer. Many treatments depend on the localization of cancer within the prostate to appropriately target treatment to the cancerous cells while sparing healthy tissue. Imaging is especially important for the treatment of advanced disease, as rapid detection of cancer that has spread outside the prostate (metastasis) allows patients to begin treatments earlier and increases the odds that patients will receive treatment within the optimal therapeutic window. There are many types of images used to detect and diagnose prostate cancer, the most common imaging techniques are discussed below:
Transrectal Ultrasound (TRUS):
This technique uses a small probe inserted into the rectum to send sound waves into the prostate. The echo of the sound waves off the prostate is transformed into an image by a computer. TRUS is often used to measure the size of the prostate and as a guide for biopsy and some treatments.
Computed Tomography (CT) scan:
CT scans use x-rays to create a detailed, 3D cross-sectional image of the inside of the body. CT scans may be used to pinpoint the location of a tumor within the prostate, evaluate the extent of cancer, and assess whether the disease is responding to treatment. In some cases, CT technology is used to accurately guide cancer treatment during a procedure.
Magnetic Resonance Imaging (MRI):
MRI uses a magnetic field and radio waves to create a clear picture of the prostate. MRI can be used to locate diseased tissue within the body and to precisely pinpoint cancerous cells. MRI can also be used to see if cancer has spread outside the prostate to nearby tissues. MRI images help physicians to plan treatments such as surgery or radiation therapy.
Positron Emission Tomography (PET) imaging:
PET imaging uses a small amount of radioactive material, called a radiotracer, and a special camera to see inside the prostate. The specially designed radiotracer is injected into the patient and taken up by prostate cells, the radiotracer emits a small amount of energy which can be picked up by the PET scanner and is used to create a detailed image. This type of imaging can also identify abnormal functions in prostate cells that indicate cancer. PET Scans are usually done in combination with a CT or MRI scan.

Prostate Cancer
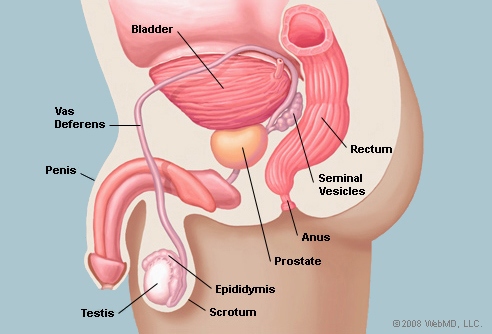
The prostate is a walnut-sized gland in men that is part of the reproductive system.
The prostate sits low in the pelvis, below the bladder, in front of the rectum and the prostate surrounds the urethra. The prostate makes seminal fluid, the liquid in sperm that protects, supports and helps transport sperm.
Prostate Cancer is the most common cancer and the second leading cause of cancer death in men.
- Over 34,000 men will die needlessly of prostate cancer.
- 1 in 8 American men will get prostate cancer in their lifetime.
- 1 in 41 men will die of this disease.
- Prostate cancer is nearly 100% survivable if caught early.
Prostate Cancer Risk Factors
Age: The risk of prostate cancer increases with age.
Genetic Mutations: Inherited mutations of the BRCA1 or BRCA2 genes raise the risk of breast, ovarian, and prostate cancer in some families.
Diet: Studies indicate there may be a link between diet and the cause or prevention of prostate cancer.
Chemical Exposure: Exposure to certain chemicals such as pesticides and herbicides may have higher than average rates of prostate cancer. Veterans who were exposed to the defoliate Agent Orange are 49% more likely than non-exposed veterans to be diagnosed with prostate cancer.
Firefighters: Recent studies show that firefighters are at a 28% greater risk to develop prostate cancer compared to the general population.
Prevalence of Prostate Cancer
About 288,300 new cases of prostate cancer will occur in the United States this year. Further, it is expected that 34,700 deaths will occur this year due to prostate cancer. This is the second leading cause of cancer death in men.
Men aged 40 and older who have at least a 10-year life expectancy should talk with their healthcare provider about having a baseline digital rectal exam of the prostate gland and a prostate-specific antigen (PSA) blood test.
Most prostate cancers are discovered in the local (confined to the prostate) stage; the 5-year relative survival rate for patients whose tumors are diagnosed at the earliest stages of the disease is nearly 100%.
What is Cancer?
Cancer is a disease characterized by the uncontrolled growth and potential spread of abnormal cells. The human body is made up of billions of cells that normally divide to reproduce themselves. Occasionally, cells abnormally divide too quickly. Rapidly dividing cells can create a mass called a tumor. Some tumors are benign (noncancerous, with no potential to spread) and others are malignant (cancerous). The growth of a benign tumor may interfere with body functions but these tumors are seldom life-threatening. On the other hand, malignant tumors invade and destroy normal tissue. By a process called metastasis, cells break away from a cancerous tumor and spread through the blood and lymphatic system to other parts of the body, where they form new tumors. Sometimes cancer grows and spreads rapidly, in other cases it develops and spreads slowly.
What is Prostate Cancer?
Prostate cancer begins when normal cells in the prostate begin to change and grow uncontrollably. Some prostate cancers grow slowly and may not cause symptoms or problems for years while other prostate cancers are more aggressive and grow quicker. Often there is no way to predict how aggressive a cancer is before a biopsy. However, there are multiple new biomarkers and genomic tests available that may aid in determining if cancer will be aggressive or not. Click below for more information about these biomarkers and genomic tests.
Prostate cancer is the most commonly diagnosed, major cancer among all Americans. The incidence of prostate cancer increases with age. Some studies have shown an overall 2-to 3-fold increase in the risk of prostate cancer in men who have a history of this disease in their families. Family history is defined as a family member such as a mother, father, brother, sister, etc. with prostate, breast, ovarian, colon, or pancreatic cancers. It is more significant if a family member was diagnosed with cancer at a younger age (less than 60 years old). The incidence rate of prostate cancer is two times higher in African-American men than in Caucasian men. Men with a BRCA1 or BRCA2 gene mutation are also at higher risk for prostate cancer.
Prostate Cancer Symptoms
In its early stages, not everyone experiences signs or symptoms of prostate cancer. However, you should go to your doctor if experience any of these symptoms because it could also be a sign of other prostate conditions.
- Problems passing urine, such as a slow or weak stream.
- Problems with needing to urine frequently, especially throughout the night.
- Problems with holding back urine or even loss of bladder control.
- Finding blood in the urine.
- Difficulty getting an erection or getting a painful erection.
- Pain in hips, lower back, and chest.
Linked with permission from the National Comprehensive Cancer Network, Inc. 2015 all rights reserved. The NCCN Guidelines for Patients and illustrations therein may not be reproduced in any form for any purpose without the express written permission of the NCCN. To view the most recent and complete version of the NCCN Guidelines for Patients, go online to NCCN.org.
Newly Diagnosed
Diagnosis & Biopsy
When prostate cancer is detected early it is nearly 100% survivable! In order to detect prostate cancer a patient will be given a PSA test and DRE from their general practitioner or urologist. If a patient has an elevated PSA test result and/or an abnormal DRE the physician may recommend a biopsy of the prostate.
In order to be diagnosed with prostate cancer a patient must have a biopsy of the prostate gland. A prostate biopsy is conducted with a transrectal ultrasound and biopsy needle to collect small slivers of prostate tissue that are analyzed for cancer. This tissue is then examined under a microscope for cancer cells. A biopsy of the prostate can be performed in the physician’s office and patients usually return home the same day.
Markers & Tests
Prostate cancer markers are making an impact on the world of prostate cancer by helping to individualize patient care in the early detection, diagnosis and treatment choices for prostate cancer. Through advanced science researchers from many different institutions and companies have developed a variety of tests that look at each persons genes or biomarkers and help to determine individual risk for having prostate cancer, the need for biopsies or repeat biopsies and often the best course of treatment.
PCEC Chairman Dr. David Crawford discusses the role of Biomarkers for Primary Care Physicians. Click here to see his article!
Click Here for the Prostate Marker Map
Markers & Tests for Early Detection of Prostate Cancer
-
PSA: Prostate-specific antigen, or PSA, is a protein produced by cells of the prostate gland. The PSA test measures the level of PSA in a man’s blood. PSA is present in small quantities in the serum of men with healthy prostates, but is often elevated in the presence of prostate cancer or other prostate disorders.
- SelectMDx: Helps identify patients at increased risk for aggressive disease, thereby aiding in the selection of men for prostate biopsy.
- phi: The Prostate Health Index (phi) is a new combination of 3 blood tests that results in a score, or “phi score.” This score gives you more accurate information on what an elevated PSA level might mean and the probability of finding cancer on biopsy.
- 4Kscore: The 4Kscore Test is a blood test that provides a patient-specific probability for finding a aggressive (Gleason score 7 or higher) prostate cancer upon biopsy. The information can be used by the Urologist to have an informed discussion with the patient about whether or not to have a prostate biopsy. The 4Kscore Test measures four prostate-specific kallikreins in the blood: Total PSA, Free PSA, Intact PSA, and Human Kallikrein 2 (hK2). The blood test results are combined in an algorithm with patient age, digital rectal exam (nodule, no nodule), and prior negative biopsy (yes, no). The 4Kscore Test then provides a % probability on a scales from <1% to >95% for the patient having aggressive prostate cancer.
- ProgensaPCA3: A FDA-approved urine test that detects the over-expression of a the PCA3 gene, which is specific to prostate cancer and an accurate predictor of whether cancer may be present. The PCA3 score is used to determine if a repeat biopsy is needed in men who are used to determine a man’s PCA3 score, which indicates the need for biopsy. Research is underway looking at PCA3 as prostate cancer screening population as well.
- ERG Protein Tissue Marker: Development of an ERG protein assays to be utilized on prostate cancer biopsy tissue is also underway. Presence of the ERG protein in tissue helps to identify patients who have prostate cancer. Additionally, the presence of ERG in high grade PIN (pre-cancerous lesion) is indicative of a patient more likely to be diagnosed with cancer upon the next biopsy.
Markers & Tests for Determining Who to Repeat Biopsy
- ConfirmMDx: For men with an initial negative biopsy, independently published clinical studies have shown that the ConfirmMDx test is the most significant, independent predictor of patient outcome relative to other available clinical factors such as age, PSA and DRE results.
- PCA3: If you are concerned about prostate cancer because of an elevated PSA or are feeling insecure about a previously performed (negative) biopsy, the PCA3 urine test can provide additional information that may help you and your physician to decide whether a (new) biopsy is really needed.
- 4Kscore: The 4Kscore Test is a blood test that provides a patient-specific probability for finding a aggressive (Gleason score 7 or higher) prostate cancer upon biopsy. The information can be used by the Urologist to have an informed discussion with the patient about whether or not to have a prostate biopsy. The 4Kscore Test measures four prostate-specific kallikreins in the blood: Total PSA, Free PSA, Intact PSA, and Human Kallikrein 2 (hK2). The blood test results are combined in an algorithm with patient age, digital rectal exam (nodule, no nodule), and prior negative biopsy (yes, no). The 4Kscore Test then provides a % probability on a scales from <1% to >95% for the patient having aggressive prostate cancer.
Markers & Tests for Determining Who to Treat for Prostate Cancer
- Oncotype DX: The Oncotype DX Prostate Cancer Assay harnesses the power of genomics to provide a more precise and accurate assessment of risk based on individual tumor biology.
- Prolaris: Prolaris is a measure of how fast a prostate cancer tumor is growing. Biopsy tissue samples can be used to determine a patient’s personal Prolaris Score. Studies have shown that Prolaris provides an accurate assessment of cancer aggressiveness.
- P10: "Most studies have found that PTEN loss is a powerful predictor of which prostate tumors are likely to recur or metastasize," says urologic pathologist Tamara Lotan, M.D.
- ProMark: On September 10, 2013, Metamark announced positive results from a large clinical validation study of ProMarkTM, its biopsy-based prostate cancer prognostic test. The study met its primary endpoint demonstrating that ProMarkTM, evaluated in standard formalin-fixed, paraffin-embedded prostate tissue, can differentiate indolent from aggressive disease.
Markers & Tests for Determining Who Would Benefit from Additional Treatment
- Prolaris: Prolaris is a measure of how fast a prostate cancer tumor is growing. Biopsy tissue samples can be used to determine a patient’s personal Prolaris Score. Studies have shown that Prolaris provides an accurate assessment of cancer aggressiveness.
- Decipher: The Decipher test predicts the probability of metastasis after surgery and provides an independent assessment of tumor aggressiveness; information distinct from that provided by Gleason score or PSA.
Markers & Tests for Ongoing Testing
- PSA: Prostate-specific antigen, or PSA, is a protein produced by cells of the prostate gland. The PSA test measures the level of PSA in a man’s blood. PSA is present in small quantities in the serum of men with healthy prostates, but is often elevated in the presence of prostate cancer or other prostate disorders.
- Testosterone: In men, testosterone plays a key role in the development of male reproductive tissues such as the testis and prostate as well as promoting secondary sexual characteristics such as increased muscle, bone mass, and the growth of body hair.
- Circulating Tumor Cells: Circulating tumor cells (CTCs) are cells that have shed into the vasculature from a primary tumor and circulate in the bloodstream. CTCs thus constitute seeds for subsequent growth of additional tumors (metastasis) in vital distant organs, triggering a mechanism that is responsible for the vast majority of cancer-related deaths.
Markers & Tests for Genetic Testing
- Genetic Testing: Genetic counseling before and after genetic testing is very important. Genetic testing plays an important role in identifying who is at risk for certain disease, who is at risk for more aggressive disease and often genetic testing can play a critical role in determining the best and most effective treatment options. In prostate cancer specifically, identifying genetic mutations of inherited prostate cancer has implications for a man's risk of prostate cancer, the risk of more aggressive disease and to personalize treatment options. Additionally, there may be an impact on families, if certain gene mutations are found it may be important that family members are also tested.
To learn more about Prostate Cancer Markers, visit www.prostatemarkers.org
Advanced Disease
Four Categories of Advanced Prostate Cancer [AIPC]
Advanced prostate cancer can be classified into four disease categories ranging from advanced prostate cancer confined to the prostate gland to prostate cancer that has spread to lymph nodes and bones.
1. Locally Advanced Prostate Cancer
Cancer that has grown to fill the prostate or has grown through the prostate and may extend into the glands that help produce semen (seminal vesicles), or the lymph nodes. Occurs in men who have been treated for early prostate cancer, but their PSA is rising. A bone scan and CAT scan in these patients is usually shows no evidence of cancer. Cancer that has grown to fill the prostate or has grown through the prostate and may extend into the glands that help produce semen (seminal vesicles), or the lymph nodes. Occurs in men who have been treated for early prostate cancer, but their PSA is rising. A bone scan and cat scan in these patients is usually shows no evidence of cancer.
2. Biochemically Recurrent Prostate Cancer (Rising PSA)
Patients who have a rising PSA after treatment, but do not have any evidence of disease spread to bone or other organs. This can occur after local treatment, or after hormone therapy. The management of such patients is controversial, and may include investigational treatments, radiation therapy, or chemotherapy.
3. Metastatic Prostate Cancer (Hormone Sensitive)
Metastatic cancer is a form of prostate cancer that has spread (metastasized) to the bone, distant lymph nodes or other parts of the body. The growth of these cancers can be controlled with treatment and depletion of the male sex hormone, testosterone, results in an improvement of tumor related symptoms such as bone pain or inability to urinate.
4. Hormone Refractory Prostate Cancer
Hormone refractory prostate cancer is also known as castration-recurrent prostate cancer or androgen-independent prostate cancer. This is a type of prostate cancer that continues to grow despite the suppression of male hormones that fuel the growth of prostate cancer cells.
A team approach is very important for this type of prostate cancer and may include a urologist, a radiation oncologist, a medical oncologist, nurses, your family, patient navigators and others.
Before a diagnosis of advanced androgen-independent prostate cancer:
- Ensure your testosterone level is zero.
- Test your PSA level several times over several months to ensure there is a consistent rise in PSA over time.
- Perhaps adding a secondary hormonal therapy to the hormonal suppression therapy you may already be taking to try and control your PSA.
Secondary hormonal therapies could include:
- Antiandrogen withdrawl (AAW)
- Antiandrogen addition (Low vs. High)
- Estrogens (I.V., oral, transdermal...)
- Ketoconazole (Nizoral)
- Aminoglutethimide (Cytadren)
- Corticosteroids
Bone Directed Therapies
When prostate cancer spreads beyond the prostate, it usually spreads to the bones first. Bone metastasis can be painful and can cause bone fractures, therefore controlling bone cancer and relieving pain and other complications is an important component of treatment. If cancer has spread to the bones, your physician may prescribe bone-directed therapies to slow cancer within the bone, reduce bone pain, and to strengthen bones.
Some drugs that are effective bone-directed therapies slow down a type of bone cell called osteoclasts. Osteoclasts normally break down the hard mineral structure of bones to help keep them healthy, however these cells can become overactive when prostate cancer spreads to the bones. These treatments can relieve bone pain, slow cancer that has spread to bones, and strengthen bones. Below is a list of common bone-directed therapies:
- Zometa (Zoledronic Acid)
- Xgeva (Denosumab)
- Prolia (Denosumab)
Corticodteroids and radiopharmaceuticals have also been shown to be beneficial against bone pain.
Side Effects:
Some common side effects for bone-directed therapies include:
- Fatigue
- Bone or joint pain
- Nausea
- Diarrhea
Chemotherapy Treatment
Chemotherapy is a drug treatment that uses powerful chemicals to kill fast-growing cells in your body. Chemotherapy is most often used to treat cancer, since cancer cells grow and multiply much more quickly than most cells in the body.