Incontinence
Urinary incontinence is the inability to control urination. The term may be used interchangeably with Overactive Bladder (OAB), which also includes the same frequency in urination and urinary urge. People who suffer from overactive bladder, or urinary incontinence, can't hold their urine -- they wet themselves. Leaking urine is normal only in infants; it is not a normal result of aging. If you have this problem, you may be too embarrassed or upset to ask for help. Don't be. It is estimated that over 12 million Americans have urinary incontinence. Incontinence affects all ages, both sexes, and people of every social and economic level. It is also estimated that 15 to 30 percent of people over the age of 60 who live at home have incontinence. Women are twice as likely as men to have this condition. In addition, at least half of the 1.5 million Americans who reside in nursing homes are incontinent. The exact number of people with incontinence is not known, but the total number of people affected may be far greater than current estimates.
Types of Incontinence
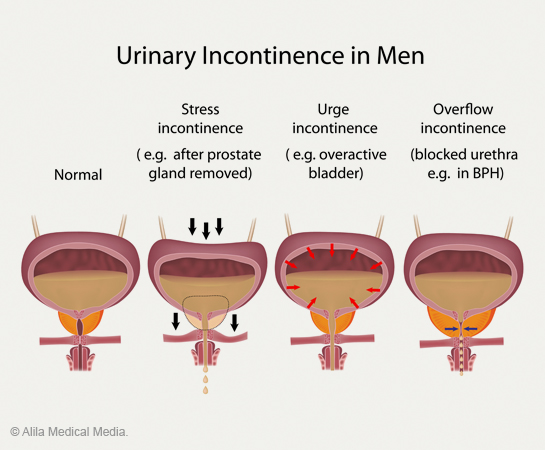
Incontinence is classified by the symptoms of or circumstances occurring at the time of urine leakage.
Stress incontinence: May be due to poor bladder support by the pelvic muscles or to a weak or damaged sphincter. This condition allows urine to leak when you do anything that strains or stresses the abdomen, such as coughing, sneezing, laughing, or even walking.
Urge incontinence: Results when an overactive bladder contracts without your wanting it to do so. You may feel as if you can't wait to reach a toilet. At times, you may leak urine without any warning at all. A bladder can become overactive because of infection that irritates the bladder lining. The nerves that normally control the bladder can also be responsible for an overactive bladder. In other cases, the cause may be unclear.
Mixed incontinence: Is often a combination of both conditions above -- stress and urge incontinence.
Overflow incontinence: Occurs when the bladder is allowed to become so full that it simply overflows. This happens when bladder weakness or a blocked urethra prevents normal emptying. An enlarged prostate can result in such blockage. For this reason, overflow incontinence is more common in men that in women. Bladder weakness can develop in both men and women, but it happens most often in people with diabetes, heavy alcohol users, and others with decreased nerve function.
Environmental incontinence (sometimes called functional incontinence): Occurs when people cannot get to the toilet or get a bedpan when they need it. The urinary system may work well, but physical or mental disabilities or other circumstances prevent normal toilet usage.
Nocturnal enuresis Is incontinence that occurs during sleep.
When individuals have two or more types of incontinence, the causes of each must be found and considered in planning appropriate treatment.
What to do about Incontinence?
The first step is to locate a health care provider, such as a urologist, who is interested in and well-informed about treating incontinence. He or she will want to become familiar with your medical history and the way in which incontinence affects you. Be sure to come prepared for your visit with: (1) a list of all the medications you are currently taking, including those you purchase without a prescription; (2) the dates and outcomes of any bladder-related tests or surgical procedures you may have had; and (3) a bladder diary.
If you are seeking products to help with incontinence, click below to visit the Urology Health Store.
Prostatitis
To put it simply, prostatitis is inflammation of the prostate gland.
There are four main classifications of prostatitis
- Acute bacterial prostatitis - acute infection of the prostate gland, usually occurs in men aged 40 to 60 years. Caused by a bacterial infection and comes on suddenly. There is often blood in the urine and the PSA blood test result may be higher than normal.
- Chronic bacterial prostatitis - recurrent infection of the prostate, occurs in men aged 50 to 80 years. It is associated with chronic urinary infection and, commonly, calcifications in the prostate (prostatic stones). In the cases of bacterial prostatitis, the culprit usually is a bacteria known as Escherichia coli. The cause of bacterial prostatitis is not well defined, but one theory suggests a reflux of urine from the bladder into prostatic ducts. This reflux of urine may lead to prostatitis. The most common symptom is recurrent bladder infections.
- Chronic prostatitis - the most common yet least understood form. Found in men of any age, the symptoms include pain in the groin or bladder, and come and go without warning.
- Asymptomatic inflammatory prostatitis - this form of prostatitis has no symptoms, and is often found when undergoing tests for other conditions.
Symptoms of prostatitis
Each form of prostatitis has a slight variation in signs and symptoms.
Acute bacterial prostatitis
- Sudden onset of fever and chills
- Pain in lower back or rectum
- Irritative or obstructive urinary symptoms
- Prostate is warm, swollen, and tender upon examination
Chronic bacterial prostatitis
- Relapsing urinary tract infections
- Painful urination or other voiding problems
- Ejaculatory pain
- Pelvic or genital pain
- Some men may not have any symptoms
Chronic prostatitis
- Chronic pelvic pain (testicular, penile, lower abdominal, ejaculatory)
- Persistent inflammation of the prostate
- Absence of infectious bacteria in urine
Diagnosing prostatitis
The gold standard for diagnosing prostatitis would be to perform a biopsy of the prostate, but this is rarely done. Instead, doctors may diagnose prostatitis by examining prostatic secretions for bacteria. To do this, a "four-cup" test may be conducted. To start, the patient must have a full bladder. The doctor will clean the penis with soap and water and will then collect two cups of urine. Next, the prostate will be massaged by a digital rectal examination (DRE) to allow prostatic fluid to travel through the urethra. Two more cups of urine will be collected, and the expressed prostatic secretion (EPS) in the urine is examined for the presence of bacteria. Some physicians may not perform the "four-cup" test, and may just obtain urine before and after massaging the prostate. Sometimes EPS secretions from the urethra can be collected from the tip of the penis after massaging the prostate. After the physician collects these secretions, they can be examined under a microscope. Nonbacterial prostatitis is more difficult to diagnose. With these patients, the EPS will have evidence of inflammation, but bacteria will not be present. The lack of recurrent urinary tract infections distinguishes nonbacterial prostatitis from chronic bacterial prostatitis.
Prostate Health Conditions
